Market share trends tell you more about a company's competitive momentum than a single quarter of earnings ever could. For UnitedHealth Group (UNH), understanding its UnitedHealth market share across insurance and healthcare services is one of the clearest ways to gauge whether the company is strengthening its position or losing ground to rivals. The trajectory of that share, not just the raw number, is what matters for long-term investors doing their homework.
Key takeaways
- UnitedHealth Group is the largest private health insurer in the U.S. by enrolled membership, and its market share spans Medicare Advantage, employer-sponsored plans, and Medicaid managed care.
- Optum, UNH's healthcare services arm, has grown into a business that rivals the insurance side in revenue, giving UNH a diversified competitive moat few peers can match.
- The UNH competitive landscape includes Elevance Health (formerly Anthem), Cigna, Humana, and CVS/Aetna, each with different segment strengths.
- Total addressable market (TAM) expansion in Medicare Advantage and value-based care has been a tailwind for UNH's market position for years.
- Evaluating market share by segment, rather than in aggregate, gives a more honest picture of where UNH is winning and where it faces real pressure.
How does UnitedHealth market share break down by segment?
UNH operates across several distinct insurance and services markets, and lumping them together masks important differences. The company's insurance business, housed under UnitedHealthcare, covers employer-sponsored (commercial) plans, Medicare Advantage, Medicaid managed care, and individual exchange plans. Optum, the services side, covers pharmacy benefit management (through OptumRx), healthcare delivery (OptumHealth), and data/analytics (OptumInsight).
In Medicare Advantage alone, UNH has historically held the largest share of any single insurer, typically enrolling a substantial portion of all MA beneficiaries nationwide. Humana has been the closest competitor in MA, while Elevance Health and CVS/Aetna trail behind. In commercial insurance, the picture is more fragmented. Large national carriers like Elevance, Cigna, and Aetna all hold meaningful shares, and regional Blue Cross Blue Shield affiliates collectively control a large chunk of the employer market. UNH leads nationally, but the gap is narrower here than in Medicare Advantage.
Medicare Advantage (MA): A type of Medicare plan offered by private insurers as an alternative to Original Medicare. MA plans often bundle hospital, medical, and prescription drug coverage. The MA market has been growing as a share of total Medicare enrollment for over a decade, which matters because it expands the addressable market for insurers like UNH.
On the Optum side, market share is harder to pin down because the business competes across pharmacy services, physician practices, ambulatory surgery centers, and health IT. OptumRx is one of the three largest pharmacy benefit managers alongside CVS Caremark and Express Scripts (owned by Cigna). OptumHealth has been aggressively expanding its network of employed and affiliated physicians, making it one of the largest physician practice groups in the country.
What is UNH's market position in Medicare Advantage?
Medicare Advantage is where UNH's dominance is most visible. The company has consistently enrolled more MA members than any other insurer. To put this in perspective, UNH and Humana together typically account for roughly half of all MA enrollment nationwide. That concentration gives UNH significant leverage with providers and scale advantages in plan design and pricing.
The MA market itself has been expanding. The share of Medicare-eligible Americans choosing MA over Original Medicare has been climbing steadily, from roughly a third of beneficiaries a decade ago to approaching half or more in recent years. That growing TAM has allowed multiple insurers to add members simultaneously, but UNH has generally grown at or above the overall market rate, which means its share has either held steady or ticked up.
Humana, traditionally UNH's closest MA rival, is heavily concentrated in this segment. Elevance Health and CVS/Aetna have been investing to grow their MA books but from a smaller base. The competitive dynamic here is worth watching because CMS (Centers for Medicare and Medicaid Services) Star Ratings directly affect plan economics. A ratings downgrade can force an insurer to reduce benefits or absorb margin compression, which reshuffles competitive positioning from year to year.
How does the UNH competitive landscape look in commercial insurance?
Commercial insurance, meaning employer-sponsored and individual plans, is a messier picture. UNH is the largest single national carrier by membership, but the market is far more fragmented than MA. Blue Cross Blue Shield licensees, operating independently across different states, collectively hold the largest combined share of the commercial market. When you compare UNH head-to-head against any single BCBS affiliate, UNH is larger. But the BCBS network as a whole is a formidable competitor.
Elevance Health (which operates as Anthem and several BCBS-branded plans) is UNH's most direct national competitor in this segment. Cigna and Aetna round out the top tier. The competitive dynamics in commercial insurance depend heavily on geography, employer size, and network breadth. A carrier might dominate in one state and barely register in another.
For investors evaluating UnitedHealth industry share in commercial lines, the key question is whether UNH is winning new large employer accounts and retaining existing ones. Retention rates and new business wins in the large group market are better indicators of competitive health than headline membership numbers, which can swing with a single large account gain or loss.
Why does Optum change the UnitedHealth market share story?
Here is the thing about analyzing UNH purely as an insurer: you miss half the company. Optum has grown from a supporting business into a revenue engine that, by some measures, now generates more revenue than UnitedHealthcare itself. That matters for market share analysis because Optum competes in entirely different markets than the insurance arm.
OptumRx competes with CVS Caremark and Express Scripts in pharmacy benefit management. OptumHealth competes with hospital systems, physician groups, and other care delivery organizations. OptumInsight competes with health IT companies and consulting firms. In each of these, UNH has been gaining ground through a combination of organic growth and acquisitions.
Vertical integration: A strategy where a company controls multiple stages of its supply chain. For UNH, this means owning both the insurance side (paying for care) and the services side (delivering care). Vertical integration can create cost advantages, but it also raises questions about conflicts of interest that investors should consider.
The vertical integration between UnitedHealthcare and Optum is one of UNH's biggest competitive advantages and also one of its most debated features. By routing members to Optum-owned clinics and pharmacies, UNH can capture margin at multiple points. Competitors like Cigna (which owns Express Scripts) and CVS Health (which owns Aetna) have pursued similar strategies, but UNH's scale in care delivery through OptumHealth is arguably the broadest.
If you want to dig deeper into UNH's business segments and financials, reviewing the breakdown of revenue and operating earnings by segment is a good starting point.
Is UNH gaining or losing ground versus Elevance and Cigna?
This depends on the segment. In Medicare Advantage, UNH has generally maintained or grown its lead. Elevance and Cigna have been growing their MA books, but from a smaller base, so UNH's absolute share advantage has been hard to close. Humana remains the more relevant MA competitor.
In commercial insurance, the picture is more competitive. Elevance has strong regional positions through its BCBS licenses and has been investing in technology and value-based care arrangements. Cigna, after merging with Express Scripts, has leaned into its PBM and specialty pharmacy capabilities to differentiate on cost management for employers. Both are credible competitors for large national accounts.
In healthcare services, UNH's Optum has been the most aggressive acquirer and builder. Cigna's Evernorth (which includes Express Scripts) competes well in PBM and specialty pharmacy, but lacks Optum's breadth in care delivery. Elevance's Carelon health services division is growing but remains smaller in scale.
The honest assessment: UNH's overall UNH market position has strengthened over the past several years relative to each individual competitor. But the gap varies meaningfully by segment, and no single rival is weak across the board.
What is the total addressable market and why does it matter?
Understanding TAM helps you evaluate whether UNH's market share gains are coming from a growing pie or from taking slices away from competitors. In most of UNH's key markets, the pie has been growing.
- Medicare Advantage: The aging U.S. population and increasing MA penetration rates have expanded this market substantially. More people aging into Medicare, combined with more of them choosing MA plans, creates a compounding growth dynamic.
- Medicaid managed care: State-by-state expansion of managed Medicaid has opened new markets for national insurers, though Medicaid margins are thinner and more politically sensitive.
- Healthcare services: The shift toward value-based care, where providers are paid for outcomes rather than volume, has expanded the addressable market for companies like Optum that can manage risk and coordinate care.
- Pharmacy benefits: Rising drug costs and specialty pharmacy growth have increased the importance and revenue pool for PBMs.
When TAM is expanding, a company can grow revenue without necessarily taking share from competitors. But if UNH is growing faster than the market, that combination of TAM expansion plus share gains is a strong competitive signal. Conversely, if a competitor's growth merely matches market growth, their share is effectively flat even if their membership numbers look good.
How to evaluate UnitedHealth market share as an investor
If you are researching UNH's competitive position, here is a practical framework:
- Segment the analysis. Look at MA, commercial, Medicaid, and Optum separately. Aggregate numbers hide the real story.
- Compare growth rates, not just absolute size. A company growing membership at twice the market rate is gaining share even if it is not the largest player.
- Watch Star Ratings in MA. CMS Star Ratings affect bonus payments and plan attractiveness. A ratings change can shift competitive dynamics quickly.
- Track Optum's revenue mix. The split between external and internal (intercompany) Optum revenue tells you how much of Optum's growth comes from the captive UnitedHealthcare channel versus winning outside clients.
- Monitor medical loss ratios (MLRs). A rising MLR can indicate pricing pressure or higher utilization, both of which affect competitive positioning over time.
Medical Loss Ratio (MLR): The percentage of premium revenue an insurer spends on medical claims and quality improvement. An MLR of 85% means 85 cents of every premium dollar goes to care. Lower MLRs mean more margin for the insurer, but regulators set minimum MLR thresholds.
You can run this kind of competitive screening across health insurers to compare growth rates and profitability metrics side by side. Pair that with a look at the stock analysis framework for evaluating individual positions.
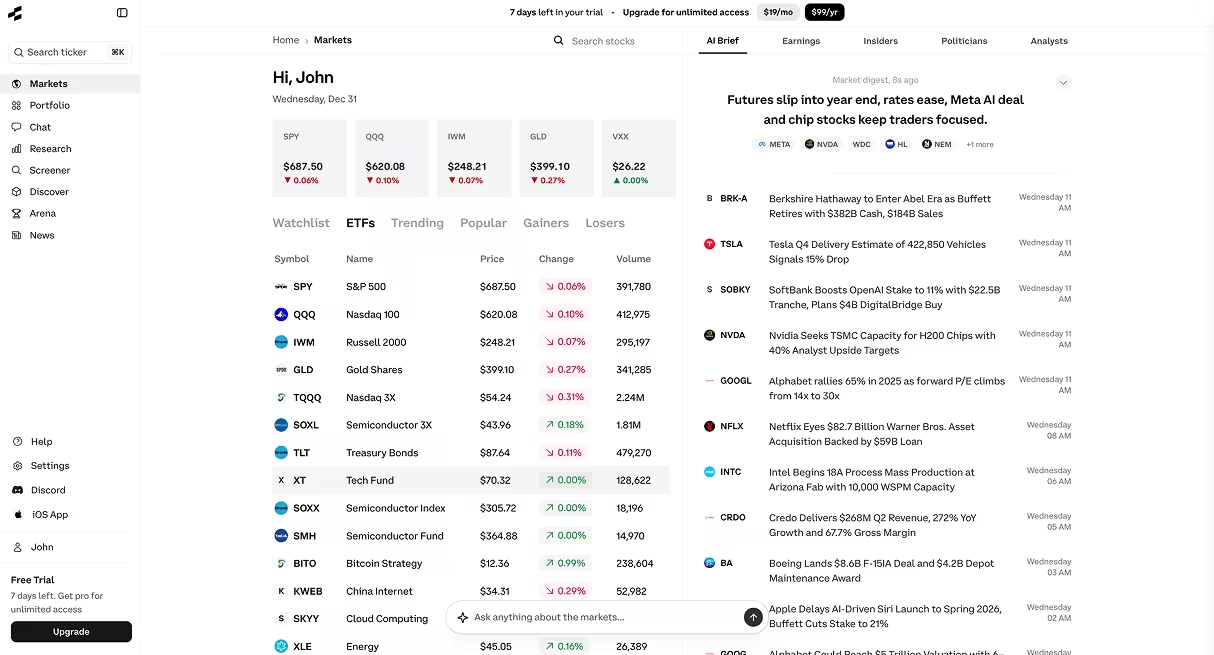
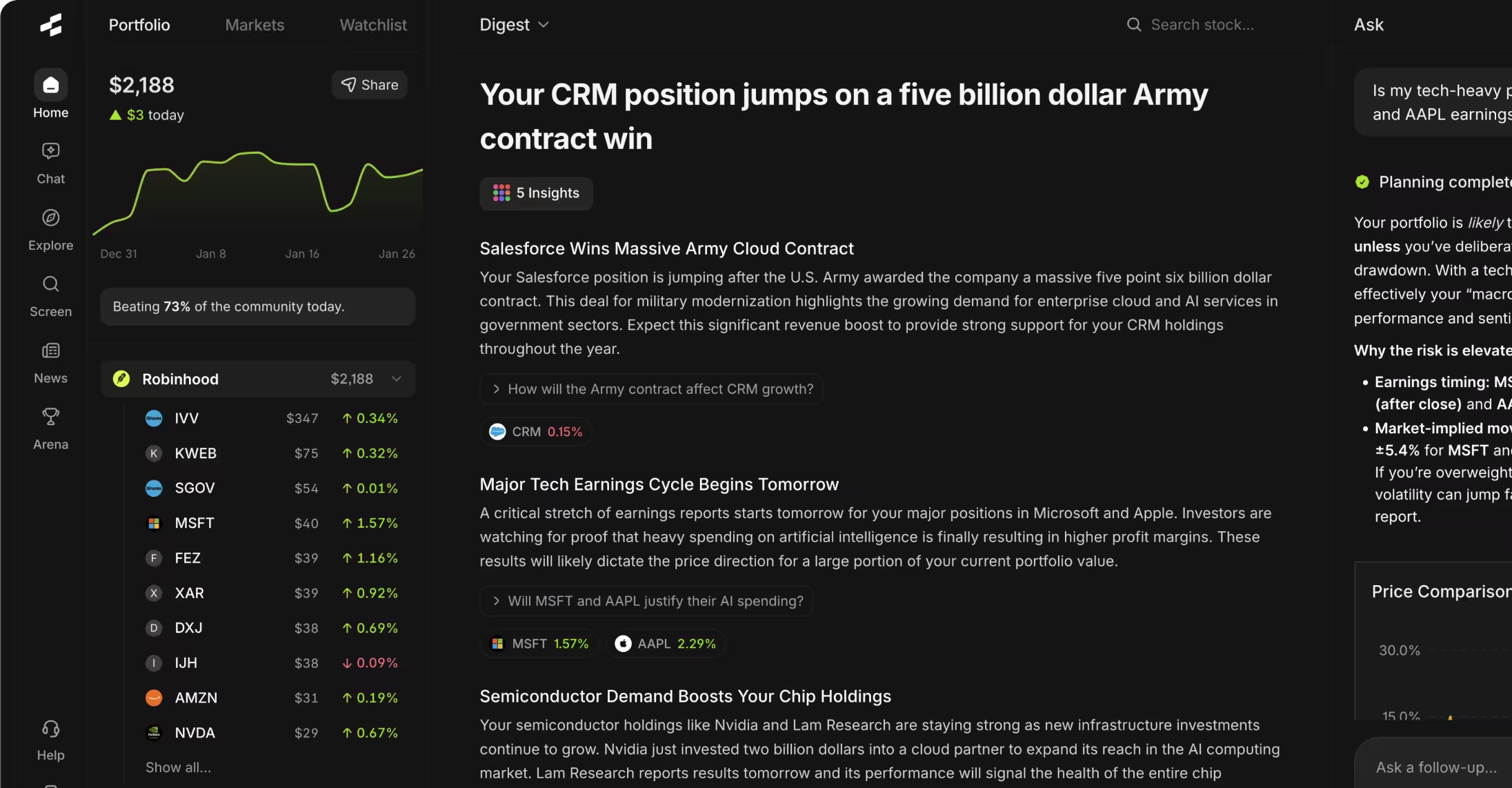
Try it yourself
Want to run this kind of analysis on your own? Copy any of these prompts and paste them into the Rallies AI Research Assistant:
- How does UNH's market share break down across Medicare Advantage, commercial insurance, and Optum services — and how has their competitive position in each segment changed over the last few years compared to Anthem and Cigna?
- What's UnitedHealth's market share in its core markets? Is it gaining or losing ground?
- Compare UNH, ELV, CI, and HUM across Medicare Advantage enrollment growth, commercial retention, and healthcare services revenue as a percentage of total revenue.
Frequently asked questions
What is UnitedHealth's market share in Medicare Advantage?
UnitedHealth Group has historically held the largest share of Medicare Advantage enrollment among individual insurers. Along with Humana, the two companies typically account for roughly half of all MA enrollees. The exact percentage shifts year to year based on plan bids, Star Ratings, and member choices during open enrollment periods.
How does the UNH competitive landscape differ by segment?
In Medicare Advantage, UNH's primary competitor is Humana. In commercial insurance, UNH competes most directly with Elevance Health, Cigna, and the Blue Cross Blue Shield network of affiliates. In healthcare services, Optum competes with CVS Caremark and Express Scripts in pharmacy benefits, and with hospital systems and physician groups in care delivery. Each segment has its own competitive dynamics.
Is UnitedHealth industry share growing or shrinking?
Broadly, UNH has been gaining or maintaining share across most segments. The Medicare Advantage and healthcare services markets have been expanding, and UNH has generally grown at or above market rates. Commercial insurance is more competitive and fragmented, so share gains there are more incremental.
What role does Optum play in UNH's market position?
Optum is a major part of UNH's competitive advantage. It provides pharmacy benefits, healthcare delivery, and data analytics, generating revenue that in some periods exceeds the insurance arm. Optum's vertical integration with UnitedHealthcare creates cost efficiencies that are difficult for less diversified competitors to replicate.
How do Star Ratings affect UnitedHealth market share in Medicare Advantage?
CMS Star Ratings determine bonus payments that insurers receive for high-quality MA plans. Higher-rated plans can offer richer benefits, which attracts more members. A downgrade can force benefit reductions that push members to competitors. Star Ratings are one of the most direct levers affecting year-over-year MA market share shifts.
How does UNH compare to CVS/Aetna as a vertically integrated health company?
Both companies own insurance and healthcare services businesses. CVS Health combines Aetna (insurance), CVS Caremark (PBM), and CVS retail pharmacies. UNH pairs UnitedHealthcare with Optum. UNH's care delivery footprint through OptumHealth is broader than CVS's clinical operations, while CVS has a larger retail pharmacy presence. The strategies overlap but differ in emphasis.
Bottom line
UnitedHealth market share is best understood segment by segment. In Medicare Advantage, UNH is the clear leader with a durable scale advantage. In commercial insurance, it leads nationally but faces meaningful competition from Elevance, Cigna, and BCBS affiliates. Optum adds a diversified services business that most competitors have not matched in breadth. The overall trend has favored UNH, but the degree of that advantage varies by market.
If you want to build a more complete picture of UNH's competitive position and how it fits into a broader stock analysis framework, start by breaking the business into its component segments and evaluating each on its own terms. That is where the real insight lives.
Disclaimer: This article is for educational and informational purposes only. It does not constitute investment advice, financial advice, trading advice, or any other type of advice. Rallies.ai does not recommend that any security, portfolio of securities, transaction, or investment strategy is suitable for any specific person. All investments involve risk, including the possible loss of principal. Past performance does not guarantee future results. Before making any investment decision, consult with a qualified financial advisor and conduct your own research.
Written by Gav Blaxberg, CEO of WOLF Financial and Co-Founder of Rallies.ai.